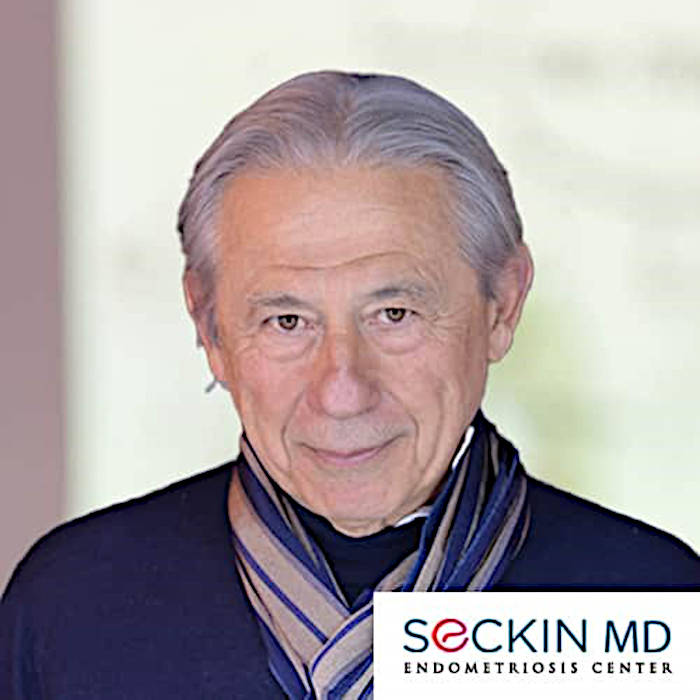
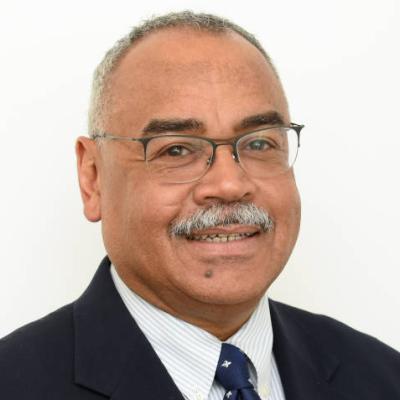
Michael Barone, MD, MPH
National Board of Medical Examiners (NBME)
Philadelphia, PA
Michael Barone is Vice President, Competency-Based Assessment at NBME in Philadelphia, PA, where he focuses on the assessment of skills and behavioral competencies for medical practice. He is a pediatrician and medical educator and completed his residency and chief residency in pediatrics at Johns Hopkins Hospital, and a Master of Public Health at the Johns Hopkins School of Hygiene and Public Health. Michael has served in various previous leadership roles, including Vice President for Licensure Programs at NBME, and Director of Medical Student Education, Assistant Dean for Student Affairs, and Associate Dean for Faculty Educational Development at the Johns Hopkins University School of Medicine. He continues to teach and mentor at Johns Hopkins as an Adjunct Associate Professor of Pediatrics.