Introduction to Diagnostic Excellence
- x

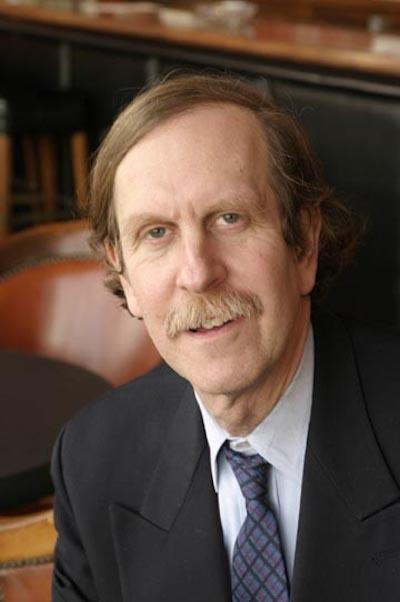
Mark Graber, MD, FACP
FounderSociety to Improve Diagnosis in MedicineDr. Graber is Professor Emeritus at Stony Brook University. He has an extensive background in biomedical and health services research, with over 150 peer-reviewed publications. He originated Patient Safety Awareness Week in 2002, an event now recognized internationally. He is the 2014 recipient of the John M Eisenberg Award for Patient Safety and Quality, awarded by The Joint Commission and the National Quality Forum, the nation's top honor in the field of patient safety. Dr. Graber has been a pioneer in efforts to address diagnostic errors in medicine, and his academic work in this area has been supported by the National Patient Safety Foundation, the Agency for Healthcare Research and Quality, and the Office of the National Coordinator for Health Information Technology. He convened and chaired the first Diagnostic Error in Medicine conference in 2008, and in 2011 he founded the Society to Improve Diagnosis in Medicine (SIDM), and served as President from 2011 through 2018.
- x
Gordon Schiff, MD
Associate DirectorBrigham and Women’s Center for Patient Safety Research and Practice
Boston, MADr. Schiff is a practicing general internist and Associate Director of Brigham and Women’s Center for Patient Safety Research and Practice, and Quality and Safety Director for Harvard Medical School (HMS) Center for Primary Care.
He has published widely in areas of medication and diagnosis safety. He was a reviewer and contributor to the 2015 National Academy of Medicine Report Improving Diagnosis in Health Care. He chairs editorial board of Medical Care. He has authored more than 200 papers and chapters including several recent papers detailing conservative prescribing and diagnosis practices as ways to transform unsafe and costly use of drugs and diagnostic testing.
He is recipient of the Institute for Safe Medication Practices Lifetime Achievement Award in 2006, the 2019 Mark Graber Diagnosis Safety Award by the Society for Improving Diagnosis in Medicine (SIDM), and in 2020 John Eisenberg Award by the National Quality Forum and the Joint Commission.
This session targets ‘first timers’ at SIDM conferences and anyone interested in a general introduction to diagnostic quality and safety: where it’s been, where it is now, and where it’s headed next.
Presented by 3 leaders in this field, the session will include:
- A short history of SIDM and the field, and how you can be involved;
- An overview of diagnostic error; cognitive and system-related contributing factors;
- An introduction to diagnostic excellence – what it is and how to achieve it;
- An introduction to pitfalls in diagnosis, and “don’t miss” conditions;
- Take home points – things you could do tomorrow in your own practice setting.
Learning Objectives:
- Acquire a working understanding of the diagnostic error field, where it’s been, where it is now, and where its headed next;
- Gain the ability to define diagnostic error, identify cases of error, and dissect out root causes;
- Discover ideas for how quality can be improved generally, and in one’s one practice.
Disparities in Diagnosis and Treatment: Equity Through Education
- x

Samantha Wang, MD
Clinical Assistant ProfessorStanford University
Stanford, CASamantha Wang is an Assistant Professor in the Department of Medicine at Stanford University and a practicing hospitalist. She graduated from Stanford Internal Medicine residency and completed a Chief Resident year followed by a Rathmann Family Fellowship in Medical Education. Her scholarly interests include creating, implementing, and assessing educational innovations throughout the continuum of medical education with a focus on health equity and anti-racism. Her research uses mixed methods, including community-based participatory research and qualitative methods to study and promote teaching health equity to clinical learners. She has been recognized regionally and nationally for her contributions to the field of diversity, equity, and inclusion.
Implicit bias and structural racism affect the way clinicians evaluate, diagnose, and treat patients, and directly contributes to health inequities and poor health outcomes. In training, students and residents encounter teachable moments in recognizing and addressing health inequities. However, teaching on this topic in clinical decision making is rarely done due to clinician reported barriers of lack of time, knowledge, expertise, authority, and fear of creating discomfort.
This interactive workshop will guide participants through common examples of structural racism and implicit bias affecting everyday medical decision-making. Topics covered will include scientific racism, use of race coefficients in clinical calculators, implicit bias in diagnosis and management, and adverse events when caring for patients with limited English proficiency. Each case will discuss the historical roots of bias in current standards of practice and provide recommendations on resources or concrete steps to practice more equitably.
Participants will then be introduced to a published teaching framework, the 5-Minute Moment for Racial Justice, as a resource to navigate these teaching moments. Participants will practice language and content in role play scenarios to normalize discussions around anti-racism with clinical learners. Learners of all backgrounds will leave with concrete tools and skills to teach peers, trainees, and students to teach antiracism effectively and concisely across all clinical settings.
Learning Objectives
- Recognize that race is a social construct and racism contributes to health disparities;
- Identify how bias and structural racism affect clinical decision making;
- Create 3 scripts of useful phrases to teach anti-racism and promote health equity with learners.
Navigating the Complexities and Uncertainties in Diagnosis from a Cognitive Psychology Lens
- x

Laura Zwaan, PhD
Assistant ProfessorErasmus MC
Institute of Medicinal Education Research Rotterdam (iMERR)
Rotterdam, The NetherlandsLaura Zwaan, PhD is an Assistant Professor at the Institute of Medical Education Research Rotterdam (iMERR) of the Erasmus MC in Rotterdam. She is a cognitive psychologist and epidemiologist who dedicates her career to understanding and improving the diagnostic process. She is committed to create awareness for the topic of diagnostic error in medicine. Laura initiated the European Diagnostic Error in Medicine conferences and was the main organizer and chair of the 1st European conference in Rotterdam in 2016 and the co-chair for the conference in Bern, Switzerland (2018). Dr. Zwaan is an active member of the Society to Improve Diagnosis in Medicine (SIDM) and has been on the scientific committee for the Diagnostic Error in Medicine conferences for 8 years (2011-2018) and she served as the chair of the SIDM research committee (2015-2017).
- x

Andrew Olson, MD
Associate Professor of Medicine and PediatricsUniversity of Minnesota
Minneapolis, MNDr. Andrew Olson is an Associate Professor of Medicine and Pediatrics at the University of Minnesota Medical School, where he practices hospital medicine and pediatrics. He serves as the founding Director of the Division of Hospital Medicine within the Department of Medicine. Dr. Olson presently serves as the Director of Medical Education Research and Innovation in the Medical Education Outcomes Center, focusing on linking education with clinical and workforce outcomes. Dr. Olson's academic work focuses on the nature and development of clinical reasoning as well as methods to measure and decrease diagnostic error.
- x

Jenny Sloane, MS, PhD
HRS Postdoctoral FellowUS Dept. of VA and Baylor College of MedicineI’m a postdoc fellow in Health Services Research and Development at the Center for Innovations in Quality, Effectiveness and Safety, which is associated with the Houston VA and Baylor College of Medicine. I received my PhD in cognitive psychology from University of New South Wales. My research interests include improving diagnostic decision-making, reducing errors in medicine, and studying the effects of interruptions and time-pressure on decision-making.
“Medicine is a science of uncertainty and an art of probability” - William Osler
The diagnostic process is complex, and many diagnostic decisions are made under uncertainty. How are these decisions made? How do physicians manage uncertainty? Are there any strategies for managing and communicating uncertainty? How do members of the health care team construct a shared mental model of uncertainty with patients and their families?
This interactive workshop focuses on exploring uncertainty in the diagnostic process from a cognitive psychology perspective and how this applies to the clinical environment. We will first discuss an overview of cognitive processes involved in diagnosis, how frameworks of cognition can help us understand clinical reasoning and why errors may occur, and the role of metacognition in improving diagnostic performance. We will also discuss how emerging theories such as social cognitive theories impact clinical reasoning, especially among teams.
Then we will explore the concept of uncertainty, with discussions on the tolerance of uncertainty in diagnosis and practical strategies to manage and communicate uncertainty in clinical practice. This will be an engaging and interactive workshop, featuring polls and clinical cases to stimulate rich discussion.
Learning Objectives:
- Understand the diagnostic process from a cognitive psychology perspective;
- Navigate the role of uncertainty in diagnostic decision-making;
- Identify practical strategies to manage and communicate uncertainty as well as create shared understanding.







